 Medical professionals are expected to uphold a standard of care in their practice. Unfortunately, life can present us with unfortunate circumstances where this standard is not met. When we experience injuries or worse due to the actions of those responsible for our treatment, healing, or diagnosis, medical malpractice claims can serve as a means to seek compensation and justice.
Medical professionals are expected to uphold a standard of care in their practice. Unfortunately, life can present us with unfortunate circumstances where this standard is not met. When we experience injuries or worse due to the actions of those responsible for our treatment, healing, or diagnosis, medical malpractice claims can serve as a means to seek compensation and justice.
In a recent legal battle that captured attention, a lawsuit between Randy A. Roberts, Sr., Johnson & Johnson, Inc., and its subsidiary Ethicon, Inc., took an intriguing turn. Roberts alleges that he suffered injuries caused by a defective medical device manufactured by J&J, leading him to file a product liability lawsuit. However, a district court granted summary judgment in favor of the defendants, prompting an appeal.
Roberts claims that during a hernia repair surgery in 2006, a Prolene Hernia System (PHS) produced by J&J was implanted in his body. Subsequently, he experienced debilitating pain, requiring three surgeries in 2015 to remove the PHS due to an infection. Dissatisfied with the outcome, Roberts initiated legal action against J&J, seeking damages under Louisiana law.
 The following case highlights the critical role of expert testimony in medical malpractice lawsuits and the difficulty of succeeding on such claims without it.
The following case highlights the critical role of expert testimony in medical malpractice lawsuits and the difficulty of succeeding on such claims without it. Insurance Dispute Lawyer Blog
Insurance Dispute Lawyer Blog


 Filing a medical malpractice claim in Louisiana involves navigating a complex process, including meeting strict deadlines. One crucial step is timely paying the filing fee to the Patient’s Compensation Fund Oversight Board (PCF Board). But does the “mailbox rule” apply to these payments? A recent Louisiana Court of Appeal case,
Filing a medical malpractice claim in Louisiana involves navigating a complex process, including meeting strict deadlines. One crucial step is timely paying the filing fee to the Patient’s Compensation Fund Oversight Board (PCF Board). But does the “mailbox rule” apply to these payments? A recent Louisiana Court of Appeal case,  In a significant development for medical malpractice litigation in Louisiana, the Fourth Circuit Court of Appeal recently reversed a summary judgment, underscoring the importance of thorough fact-finding and the potential need for expert testimony in such cases. The case,
In a significant development for medical malpractice litigation in Louisiana, the Fourth Circuit Court of Appeal recently reversed a summary judgment, underscoring the importance of thorough fact-finding and the potential need for expert testimony in such cases. The case,  In a recent Louisiana Court of Appeal decision, the court reinforced the importance of the
In a recent Louisiana Court of Appeal decision, the court reinforced the importance of the  A recent Louisiana Court of Appeal decision has underscored the significance of expert testimony in medical malpractice cases. The case, Mariakis v.
A recent Louisiana Court of Appeal decision has underscored the significance of expert testimony in medical malpractice cases. The case, Mariakis v. In the recent Louisiana Court of Appeal, Third Circuit, decision of
In the recent Louisiana Court of Appeal, Third Circuit, decision of 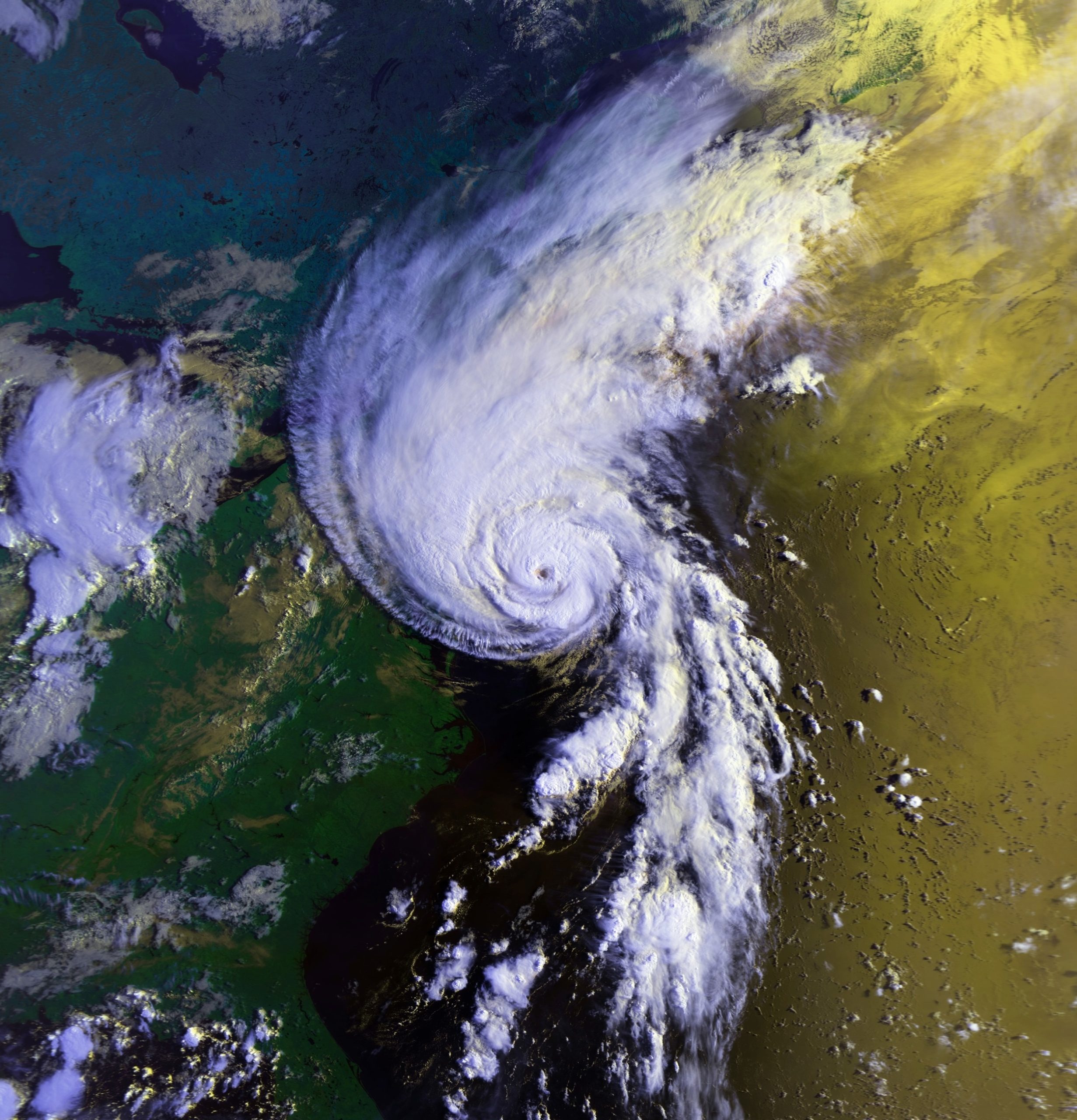 Over a decade after Hurricane Katrina, we have almost all heard of the difficult choices hospitals faced while trying to care for patients. This case involves a patient who was allegedly injured while being evacuated from a New Orleans hospital during Hurricane Katrina.
Over a decade after Hurricane Katrina, we have almost all heard of the difficult choices hospitals faced while trying to care for patients. This case involves a patient who was allegedly injured while being evacuated from a New Orleans hospital during Hurricane Katrina.  When you think about medical malpractice lawsuits, a botched surgery or missed diagnosis are likely the first things that come to mind. The following case involves a less common situation involving purported medical malpractice involving physical therapy post-surgery. It analyzes the relationship between a doctor and a physical therapist and whether a doctor can be vicariously liable for the actions of a physical therapist.
When you think about medical malpractice lawsuits, a botched surgery or missed diagnosis are likely the first things that come to mind. The following case involves a less common situation involving purported medical malpractice involving physical therapy post-surgery. It analyzes the relationship between a doctor and a physical therapist and whether a doctor can be vicariously liable for the actions of a physical therapist. A visit to the hospital is a stressful and anxious time for patients and family members. Most people, however, assume that their doctors are competent and will administer the proper standard of care. This was not the case for Richard Smallwood.
A visit to the hospital is a stressful and anxious time for patients and family members. Most people, however, assume that their doctors are competent and will administer the proper standard of care. This was not the case for Richard Smallwood.  Medical professionals are expected to uphold a standard of care in their practice. Unfortunately, life can present us with unfortunate circumstances where this standard is not met. When we experience injuries or worse due to the actions of those responsible for our treatment, healing, or diagnosis, medical malpractice claims can serve as a means to seek compensation and justice.
Medical professionals are expected to uphold a standard of care in their practice. Unfortunately, life can present us with unfortunate circumstances where this standard is not met. When we experience injuries or worse due to the actions of those responsible for our treatment, healing, or diagnosis, medical malpractice claims can serve as a means to seek compensation and justice.