 Medical malpractice claims are not always limited to instances during treatment or surgery and may, as one young patient argued, include failures that occur afterward or post-operatively.
Medical malpractice claims are not always limited to instances during treatment or surgery and may, as one young patient argued, include failures that occur afterward or post-operatively.
Justin Thomas, an eighteen-year-old, aspiring armed serviceman, underwent a right shoulder arthroscopy at Lafayette Surgicare to repair his repeated rotator cuff dislocations. The surgery was considered an outpatient procedure that Thomas’s surgeon, Dr. Otis Drew (Dr. Drew), performed beginning just before 9:00 AM on July 1, 2013, and completed around 11:00 AM the same day. Before and after the surgery, Thomas was given significant anesthesia and medication. By 1:50 PM that afternoon, Thomas was discharged into the care of his parents. Less than six hours later, after Thomas’s mom gave him a prescribed dose of oxycodone, he fell unconscious and was unresponsive to Narcan, so an ambulance arrived at Thomas’ parents’ home taking him back to the hospital, where he lay in a coma for five days. As a result, Thomas experienced brain damage and lost the use of the left side of his body.
In May 2016, a medical review board determined that despite Thomas’s injury, the medical staff, including Dr. Drew, met the required standard of care. Nevertheless, three months later, Thomas filed a lawsuit against Dr. Drew, the anesthesiologist, Lafayette Surgicare, Lafayette Surgery Center, and The Regions Health System of Acadiana. His complaint alleged that he was released too early post-operatively and prescribed extensive anesthesia and heavy narcotic medication that induced him into a coma. In response, Dr. Drew filed a summary judgment motion that the trial court, Fifteenth Judicial District Court Parish of Lafayette, granted, dismissing Thomas’s claims. Thomas appealed to Louisiana’s Third Circuit Court of Appeals (Third Circuit), arguing that the trial court erred in finding that his expert affidavit was inadmissible and did not create a genuine issue of material fact.
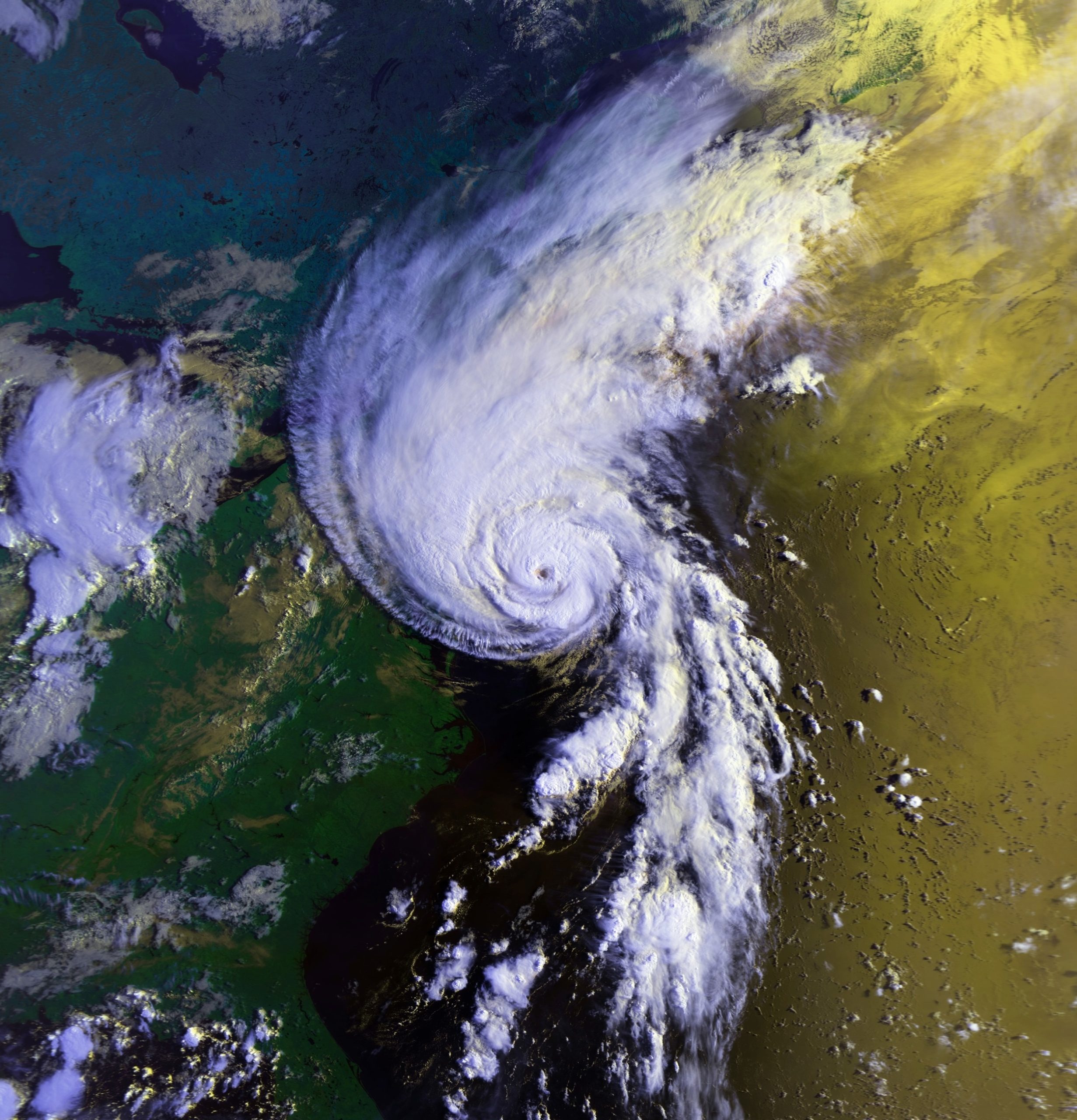 Over a decade after Hurricane Katrina, we have almost all heard of the difficult choices hospitals faced while trying to care for patients. This case involves a patient who was allegedly injured while being evacuated from a New Orleans hospital during Hurricane Katrina.
Over a decade after Hurricane Katrina, we have almost all heard of the difficult choices hospitals faced while trying to care for patients. This case involves a patient who was allegedly injured while being evacuated from a New Orleans hospital during Hurricane Katrina.  Insurance Dispute Lawyer Blog
Insurance Dispute Lawyer Blog


 When you think about medical malpractice lawsuits, a botched surgery or missed diagnosis are likely the first things that come to mind. The following case involves a less common situation involving purported medical malpractice involving physical therapy post-surgery. It analyzes the relationship between a doctor and a physical therapist and whether a doctor can be vicariously liable for the actions of a physical therapist.
When you think about medical malpractice lawsuits, a botched surgery or missed diagnosis are likely the first things that come to mind. The following case involves a less common situation involving purported medical malpractice involving physical therapy post-surgery. It analyzes the relationship between a doctor and a physical therapist and whether a doctor can be vicariously liable for the actions of a physical therapist. A visit to the hospital is a stressful and anxious time for patients and family members. Most people, however, assume that their doctors are competent and will administer the proper standard of care. This was not the case for Richard Smallwood.
A visit to the hospital is a stressful and anxious time for patients and family members. Most people, however, assume that their doctors are competent and will administer the proper standard of care. This was not the case for Richard Smallwood. 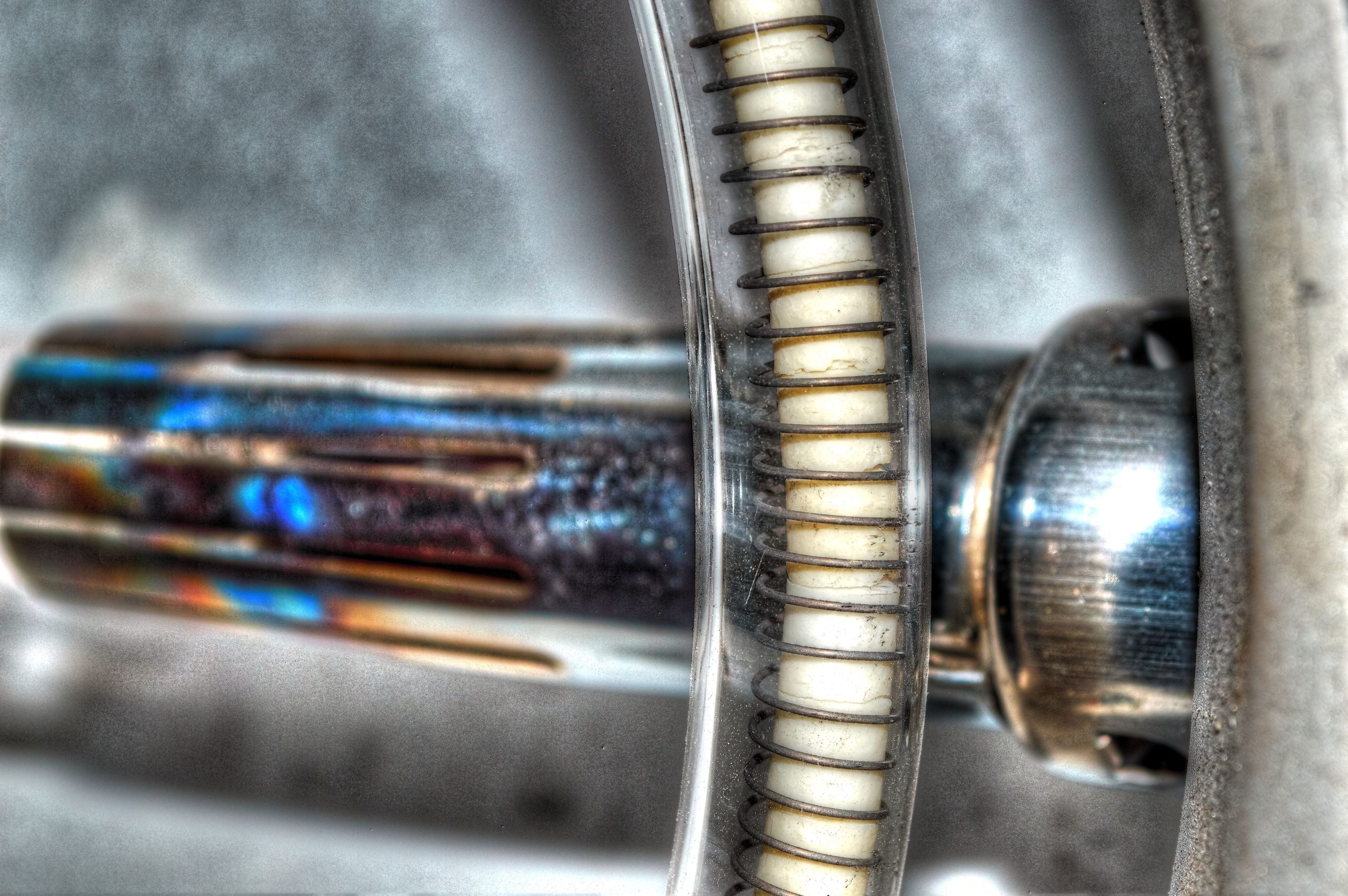 Medical professionals are expected to uphold a standard of care in their practice. Unfortunately, life can present us with unfortunate circumstances where this standard is not met. When we experience injuries or worse due to the actions of those responsible for our treatment, healing, or diagnosis, medical malpractice claims can serve as a means to seek compensation and justice.
Medical professionals are expected to uphold a standard of care in their practice. Unfortunately, life can present us with unfortunate circumstances where this standard is not met. When we experience injuries or worse due to the actions of those responsible for our treatment, healing, or diagnosis, medical malpractice claims can serve as a means to seek compensation and justice. A minor is generally unable to bring a lawsuit on their behalf. As seen in the following case, this can lead to disputes about who the proper party is to bring a lawsuit for the minor.
A minor is generally unable to bring a lawsuit on their behalf. As seen in the following case, this can lead to disputes about who the proper party is to bring a lawsuit for the minor.  Medical malpractice claims are not always limited to instances during treatment or surgery and may, as one young patient argued, include failures that occur afterward or post-operatively.
Medical malpractice claims are not always limited to instances during treatment or surgery and may, as one young patient argued, include failures that occur afterward or post-operatively.  When a patient suffers from harm done to them by the negligence of a health care provider, he may be a victim of medical malpractice. A recent Louisiana Fifth Circuit Court of Appeals case explained why it is not always a case of medical malpractice when an avoidable medical death occurs.
When a patient suffers from harm done to them by the negligence of a health care provider, he may be a victim of medical malpractice. A recent Louisiana Fifth Circuit Court of Appeals case explained why it is not always a case of medical malpractice when an avoidable medical death occurs. In the event that you find yourself in the challenging position of pursuing a medical malpractice lawsuit against your doctor, the presence of an expert witness becomes paramount. Such a witness is instrumental in establishing the negligence of your treating physician. A recent case originating from the Parish of East Baton Rouge sheds light on the specific qualifications required for expert witnesses in medical malpractice cases and the circumstances in which their testimony may be deemed unnecessary. Join us as we delve into this notable court ruling, which clarifies the vital role of experts and the instances where their expertise may be exempted.
In the event that you find yourself in the challenging position of pursuing a medical malpractice lawsuit against your doctor, the presence of an expert witness becomes paramount. Such a witness is instrumental in establishing the negligence of your treating physician. A recent case originating from the Parish of East Baton Rouge sheds light on the specific qualifications required for expert witnesses in medical malpractice cases and the circumstances in which their testimony may be deemed unnecessary. Join us as we delve into this notable court ruling, which clarifies the vital role of experts and the instances where their expertise may be exempted. Medical malpractice claims are brought when a patient is a victim of negligence at the hands of their physician. Due to the nature of this category of claims, stories of medical malpractice are often horror stories showcasing worst-case scenarios. Even further, the most intense medical malpractice claims result in the death of the patient. Understandably, the patient’s family may seek to find responsibility for the death of their loved one. In the following lawsuit, a family fails to show the legal requirements to bring a medical malpractice claim after their family member died during surgery.
Medical malpractice claims are brought when a patient is a victim of negligence at the hands of their physician. Due to the nature of this category of claims, stories of medical malpractice are often horror stories showcasing worst-case scenarios. Even further, the most intense medical malpractice claims result in the death of the patient. Understandably, the patient’s family may seek to find responsibility for the death of their loved one. In the following lawsuit, a family fails to show the legal requirements to bring a medical malpractice claim after their family member died during surgery.  While much maligned in the popular consciousness, medical malpractice lawsuits serve a vital function in protecting patients’ rights when accessing healthcare. In Louisiana, a successful medical malpractice lawsuit must show the physician being sued had a standard of care for their patient, the physician violated this standard of care, and there was a connection between this violation and the injury suffered by the patient.
While much maligned in the popular consciousness, medical malpractice lawsuits serve a vital function in protecting patients’ rights when accessing healthcare. In Louisiana, a successful medical malpractice lawsuit must show the physician being sued had a standard of care for their patient, the physician violated this standard of care, and there was a connection between this violation and the injury suffered by the patient.